
Liquid coming from your nipple
Liquid that comes from the nipple without squeezing.
Everyone has breast tissue and people of all genders can get breast cancer. This page is for people who are trans or non-binary, and anyone else who wants to know about checking and changes during transition. You can find out about breast cancer in men by visiting this page. CoppaFeel! and OUTPATIENTS have produced these resources to ensure all young people are empowered with the information they need to get to know their bodies.
OUTPATIENTS (formerly Live Through This) are the UK’s first charity dedicated to supporting and advocating for LGBTIQ+ people affected by cancer. They seek to better represent the queer community in the cancer space, working collaboratively with beneficiaries, clinicians and other organisations to drive positive outcomes for all.
We use the term ‘chest’ on this page, and ‘breast’ when we need to be clinically accurate, for example when we talk about breast cancer. You might prefer to call your chest something else, and that’s ok!
People of all ages and genders can get breast cancer. These signs may look different
on your skin tone or your body. It’s really important to know what’s normal for you. Click for more guidance on changes during transition.

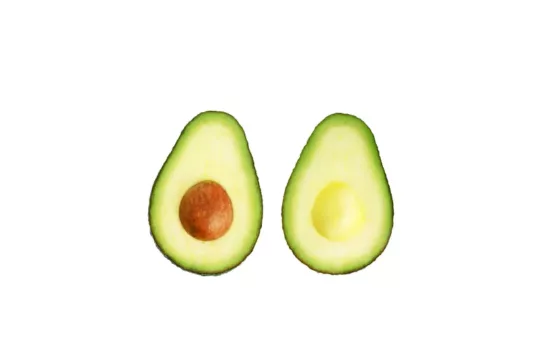
Liquid that comes from the nipple without squeezing.

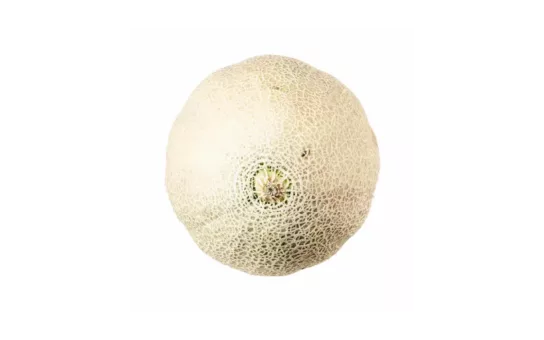
New, unusual lumps or an area that feels thicker than the rest.
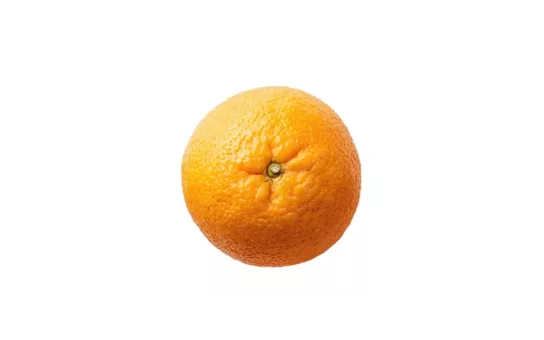
Puckering or dimpling of the skin, that might look like orange peel.
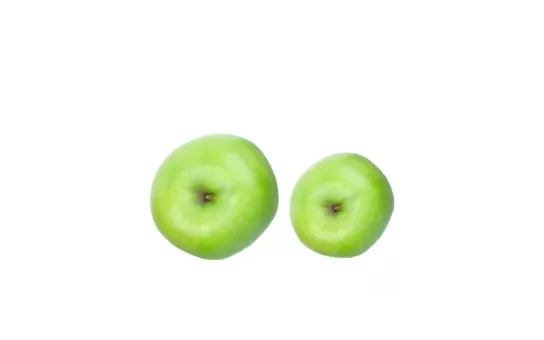
A sudden, persistent or unexplained change in size or shape.
The nipple is pointing in a different direction or is ‘pulled in’ when it’s normally out.

A lump, swelling or thickening in your upper chest or armpit area.
Redness, a rash or crusting of the nipple or the surrounding skin.
Unexplained pain that doesn’t go away with your
period (if you have them).
Breast cancer can affect people of any age or gender, so it’s really important to get to know what’s normal for your body. Everyone is
different and knowing your normal is a process, but you can start here.
If dysphoria is making this difficult, you could try
different methods, positions or settings, like checking
without a mirror, beneath loose clothing or on days
when you feel less dysphoric.
Check all parts of your chest, including your armpits, up to your collarbones and your nipples. If you have developed breasts as part of your transition, have
implants or are planning to get them this will not affect how you need to check yourself. It’s really important to
get to know your new normal.
Even if you have had top surgery, some tissue remains around the nipple, under the collarbone and in the armpit that needs to be checked – this may be referred to as ‘breast tissue’ by healthcare professionals. When
breast cancer is detected early it is more easily treated
and the survival rate is higher.
CoppaFeel! and OUTPATIENTS have worked in collaboration with our LGBTIQ+ beneficiaries to design a series of posters for Trans and Non-Binary people. Our posters give information on the signs and symptoms of breast cancer and guidance on how to check, with tips on how to get started, how to deal with dysphoria when checking, and information on how having implants or getting top-surgery might affect how you check.
OUTpatients and CoppaFeel! worked with trans and non-binary people to develop these resources. These are some of the questions that came up in the creation of these resources, and our answers to them.
We want to show the signs of breast cancer in a way that everybody can understand, whatever their body type. Some breast cancer imagery can cause dysphoria in some people, so we wanted to show something different to these typically masculine or feminine images. Signs and symptoms of breast cancer do not change, but they might vary in how they look on different bodies or skin types and colours. It is important for you to get to know what is normal for you, so that you can recognise any changes. We used fruit to show these signs and symptoms of breast cancer to avoid a ‘one size fits all’ depiction.
Breast cancer screening is for anyone between the ages of 50 and 70 who has breasts, due to either naturally-occurring oestrogen or oestrogen hormone therapy. If you are taking oestrogen you are unlikely to need breast screening in the first two years of taking it. After that, if you meet the criteria, you should think about having your breasts screened for signs of breast cancer (mammogram). If you are registered as female with your GP you should receive an automatic invite when you reach 50. If you are registered as male with your GP, you will need to request breast screening from your doctor.
It’s very common to experience changes during transition. These changes could be due to hormone treatment or surgery. Whatever the reason for the change, you will need to get to know your new normal. This can be strange at first, while you get used to the difference. Perhaps you have scar tissue or more breast tissue than before, just get to know your changes and contact your doctor if you have concerns. It is natural to feel some pain in your chest during transition, but contact your doctor if you have bad pain or unexplained changes.
Yes! Everyone needs to check. If you have had top surgery, once everything has healed, you will need to get to know your new normal by checking your chest regularly. Make sure you check areas that might still contain breast tissue. This may include tissue under your armpits and up to your collarbone, and your nipples.
You have the right to describe your body in the way you choose and your doctor should respect that. You might use the term chest, pecs, breasts, boobs, or something else, and that is fine. The doctor may at times refer to ‘breast tissue’ as this is the clinical name for the tissue that is at risk of breast cancer.
We appreciate that dysphoria can be a barrier to touching and looking at your chest. However, regular checking is important for everyone. If you’re experiencing dysphoria, try looking at your chest without using a mirror. You could also try touching your chest beneath loose clothing, or checking your chest on days when you are feeling less dysphoric. Checking might feel easier on some days than others, but getting to know what’s normal for you is a process and a practice. Keep going!
Transition is a process that can happen at any age. CoppaFeel! is a charity aimed at younger people, but this information is important and intended for every person, of any age.
You cannot have mammograms after top surgery because most of your breast tissue is removed. However, it is important that you continue to check your chest regularly. Make sure you check areas that still contain breast tissue. This might include tissue under your armpits and up to your collarbone, and your nipples. If you do need to be sent for a scan, your doctor will arrange for the right test based on your body and circumstances.
Transgender and non-binary people may use hormones to affirm their gender. According to Cancer Research UK, there isn’t enough research yet about cancer risk linked to hormone therapies used in this way.
Read more on our page about Changes during transition.
Our friends at LGBTIQ+ cancer charity OUTpatients also have some more information on hormone therapy risk.
HRT (Hormone replacement therapy) is a treatment to help with menopausal symptoms.
Menopause is when your periods stop due to lower hormone levels. It usually happens between the ages of 45 and 55, but it can happen earlier.
Breast Cancer Now talks about menopause and HRT in more detail too.
Ovarian Cancer Action talk about HRT and medical menopause in a bit more detail. Check out their FAQ section, I have a genetic mutation (BRCA1/ BRCA2/ Lynch syndrome): Can I have HRT?, and their booklet.
There is no evidence that chest binding increases your risk of breast cancer.
Top surgery is also called a mastectomy. A mastectomy is an operation to remove the breast. It can be used to treat breast cancer. Some people might have this operation to prevent breast cancer if their risk of getting breast cancer is high.
Some people decide to have top surgery as part of their transition.This is also called a bilateral mastectomy (removal of both breasts).
The word mastectomy can be used to describe surgery for breast cancer, and for transitioning.